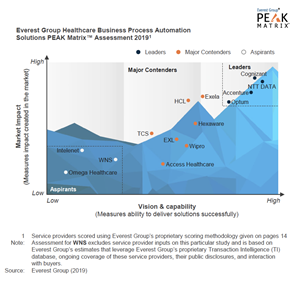
Company receives industry recognition in the latest PEAK Matrix™ for healthcare automation solutions
IRVING, Texas, Feb. 20, 2019 (GLOBE NEWSWIRE) -- Exela Technologies, Inc. (“Exela”) (NASDAQ: XELA), a location-agnostic global business process automation (“BPA”) leader across numerous industries, today announced that it has been named a Major Contender in its inaugural inclusion in Everest Group’s PEAK Matrix for Healthcare Automation Solutions in the most recent Healthcare Life Sciences Business Processing Outsourcing Market Report. According to Everest Group, a consulting and research firm focused on strategic IT, business services and sourcing, Exela holds the largest market share of the healthcare automation market, in each customer size segment. It is also one of the top four largest service providers who service both healthcare payers and providers.
|
|||||
Exela was also recognized as a Major Contender on the payer side for displaying strength in automation product development and AI-enabled solutions, for its effective implementation and integration processes and for having built most of its healthcare automation solutions in-house.
“The landscape of healthcare automation solutions is moving towards a digital future, with an emphasis on robotic process automation and artificial intelligence,” said Cisco Liquido, Vice President, Business Strategy, Exela Technologies. “We are proud to be listed in Everest Group’s PEAK Matrix, and we will continue to invest in the technologies that enhance our offerings.”
“Despite millions of dollars being spent on claims, EHR, and RCM systems, healthcare enterprises continue to lack efficiency in their existing processes. In the absence of truly end-to-end next-gen platforms, both payers and providers are resorting to automation solutions that can help bring better ROI and improve both cost and user experience,” said Manu Aggarwal, Practice Director, Everest Group. “Exela’s solutions help drive better connectivity between the payer and provider systems, thereby, streamlining the claims processing and enabling a better user experience.”
View a summary of the report and visit the Everest Group website to learn more about the PEAK Matrix assessments.
About Exela
Exela is a location-agnostic global BPA leader combining industry-specific and multi-industry enterprise software and solutions with decades of experience. Our BPA suite of solutions are deployed in banking, healthcare, insurance and other industries to support mission-critical environments. Exela is a leader in workflow automation, attended and un-attended cognitive automation, digital mailrooms, print communications, and payment processing with deployments across the globe. Exela partners with customers to improve user experience and quality through operational efficiency. Exela serves over 3,700 customers across more than 50 countries, through a secure, cloud-enabled global delivery model. We are 22,000 employees strong across the Americas, Europe and Asia. Our customer list includes 60% of the Fortune® 100, along with many of the world's largest retail chains, banks, law firms, healthcare insurance payers and providers and telecom companies.
Find out more at www.exelatech.com
Follow Exela on LinkedIn: https://www.linkedin.com/company/exela-technologies/
Follow Exela on Twitter: https://twitter.com/exelatech
Contact:
Jill Ransome, VP Marketing and Communications
E: jill.ransome@exelatech.com
T: 203-360-4555
A photo accompanying this announcement is available at http://www.globenewswire.com/NewsRoom/AttachmentNg/376ee8d9-27d1-4ff3-aaeb-5a0e1610b159
Source: Exela Technologies, Inc.